Healogics is proud to announce the launch of the Healogics Telehealth Program. The program is available immediately, providing patients access to continued wound care during Center disruptions related to COVID-19.
Learn More
Healogics Chief Medical Officer, Dr. William Ennis, assesses the impact of coronavirus on wound care patients and practice.
Learn More
The rapidly evolving COVID-19 pandemic in the United States has hospitals and acute care facilities changing standard operating procedures to prepare for the expected influx of infected patients. As a result, services, procedures, and surgeries that are deemed “non-essential” are being shut down immediately, without thorough consideration of the ramifications. The Alliance of Wound Care Stakeholders is concerned that this decision will result in unintended negative consequences that will cause a gradual influx of patients to the emergency department.
Learn More
Researchers from the University of Southern California (USC) in partnership with Healogics have recently produced a predictive model to identify wounds most likely to heal within 12 weeks. Unlike other models that have been previously published, this model utilized EMR data from over 600,000 wounds, allowing for highly predictive classification across a variety of wound types. Findings from this model also indicated that a wound’s characteristics at initial presentation, such as area, depth, and location, are far more powerful than the patient demographics or comorbidities in determining whether a wound will heal.
Learn More
Healogics Outpatient Wound Care Assessment is an audit used to determine quality improvement such as heal rates and patient access to care by measuring new patients post-Healogics management of the wound center. It is an opportunity to examine the clinical quality, operational efficiency and financial achievements of centers’ activities, as well as identify areas of potential improvement. The primary aim of this case study was to compare year-over-year center performance pre and post partnership with Healogics.
Learn More
Healogics Wound Care Centers provide exceptional wound care, but, when needed, they also want patients to receive appropriate care to treat the underlying causes of their chronic wounds. Some patients need additional care either before, during or after wound care treatment. Studies show vascular intervention can help prevent amputation and can help prevent future wounds. Whether this intervention is a revascularization consult, potential surgery or an admission, Healogics works directly with physicians to provide next steps for each patient.
To measure the impact of a Healogics collaboration for the hospital and community through understanding the continuum of care created by care delivered in the Wound Care Center, Healogics conducted an analysis across 316 Centers.
Learn More
Healogics assessed the impact of a collaborative continuum of care model between a Wound Care Center® and vascular surgery practice on quality of care and outcomes. Of the 7,616 procedures that were reviewed by Stanford Health Care’s Vascular & Endovascular Surgery practice, 1,751 procedures met inclusion criteria. This study included patients who underwent lower extremity interventions over a three-year period before and after the opening of a Wound Care Center.
Learn More
This compendium is a follow-up to the 2018 American Diabetes Association compendium Diagnosis and Management of Diabetic Foot Complications. Whereas the first compendium offered a broad general overview of diabetic foot conditions, this second volume presents a detailed discussion of the prevention and treatment of diabetic foot infections (DFIs), a major contributor to high amputation rates among people with diabetes.
Learn More
At least half of all amputations occur in people with diabetes, most commonly because of an infected diabetic foot ulcer. A thorough understanding of the causes and management of diabetic foot ulceration is essential to reducing lower-extremity amputation risk.
Learn More
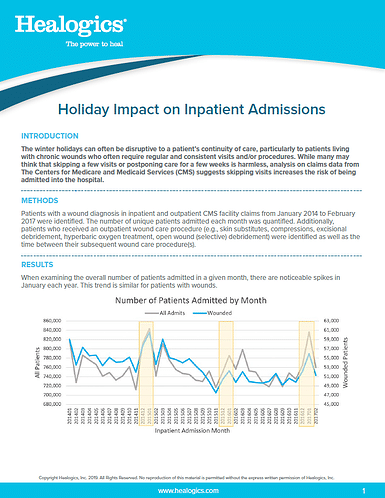
The winter holidays can often be disruptive to a patient’s continuity of care, particularly to patients living with chronic wounds who often require regular and consistent visits and/or procedures. While many may think that skipping a few visits or postponing care for a few weeks is harmless, analysis on claims data from The Centers for Medicare and Medicaid Services (CMS) suggests skipping visits increases the risk of being admitted into the hospital.
Learn More